Of all the issues we regularly see in OB/GYN medical malpractice cases, those involving uterine rupture are often the most devastating. The rupture of the uterus during pregnancy or during delivery can lead to severe and even fatal complications for both mother and child. Uterine rupture can result from a variety of complications, but the most common that we see is the weakening of the uterine wall caused by a previous cesarean section (C-section). These weaknesses are most apparent during an attempted vaginal birth after cesarean (VBAC) when the uterus is under extreme stress.

The uterus is a thick-walled hollow organ made up primarily of interlaced bundles of smooth muscle that give the uterus the ability to expand dramatically in size as the fetus develops and to contract forcefully to expel the fetus during delivery. In a C-section, the muscular wall of the uterus is cut creating a large opening to allow the surgeon to remove the fetus through an abdominal incision when the fetus fails to pass normally through the mother's pelvis. While this procedure provides a relatively safe and effective means of avoiding complications in the initial delivery, it can set the stage for increased complications in later pregnancies.

Following a C-section, the cut edges of the uterus are repaired with sutures and this incision site will heal over time, but this healing is accomplished with scar tissue, not new pristine muscle. This region of scar tissue at the original C-section site can never regain the full strength and flexibility of undamaged uterine tissue. In future pregnancies and particularly in future deliveries, when the uterus is again placed under stress by stretching and contracting, there is a substantial risk that there may be tearing or a complete rupture at the previous C-section site.

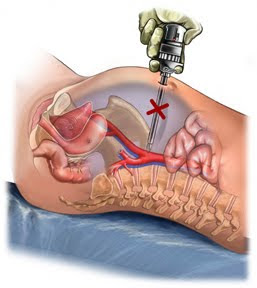
Risks of uterine rupture can affect both the mother and the fetus. For the mother, there is a risk of significant hemorrhage. The uterus is a highly vascular organ and tears can stretch and lacerate vessels of a variety of sizes. If not recognized and repaired promptly, these vascular injuries could prove fatal. For the fetus, there are a variety of risks. If the tear happens to compromise the placenta or major vessels supplying the uterus, there could be an interruption of umbilical blood flow leading to hypoxia or reduced oxygenation of the fetus. Also, if the rupture is of sufficient size, the fetus could be expelled out into the abdomen of the mother. This expulsion can also cause a partial or complete detachment of the placenta leading to a complete loss of blood supply to the fetus resulting in complete deoxygenation. An immediate diagnosis of the rupture and a repeat C-section would be necessary to rescue a fetus in such a case.

Years ago, VBAC was not an option. Any woman would delivered via C-section would never have been given the option of vaginal delivery in future pregnancies. Advances in surgical techniques and other medical practices have now made VBAC a viable option, but not all risks have been eliminated. The risks for a VBAC are significantly higher than for a normal vaginal birth. Such a delivery must be monitored closely and adequate facilities must be on hand and available to deal with any sudden emergencies. Any uterine rupture may result in devastating consequences for both mother and child.